Cognitive neuropsychiatry is a theory-driven approach to investigating psychiatric symptoms and cognitive impairments at the crossroads of psychiatry, cognitive psychology and neuroscience. Methods used are neuroimaging, computer-based cognitive tasks and psychiatric or psychological interviews or questionnaires.
Research focuses on three lines of investigation: psychiatric symptoms and vulnerability, with a focus on cognitive-emotional interactions; cognitive aging, with a focus on mild cognitive impairment; treatment and prevention, with a focus on non-invasive neurostimulation.

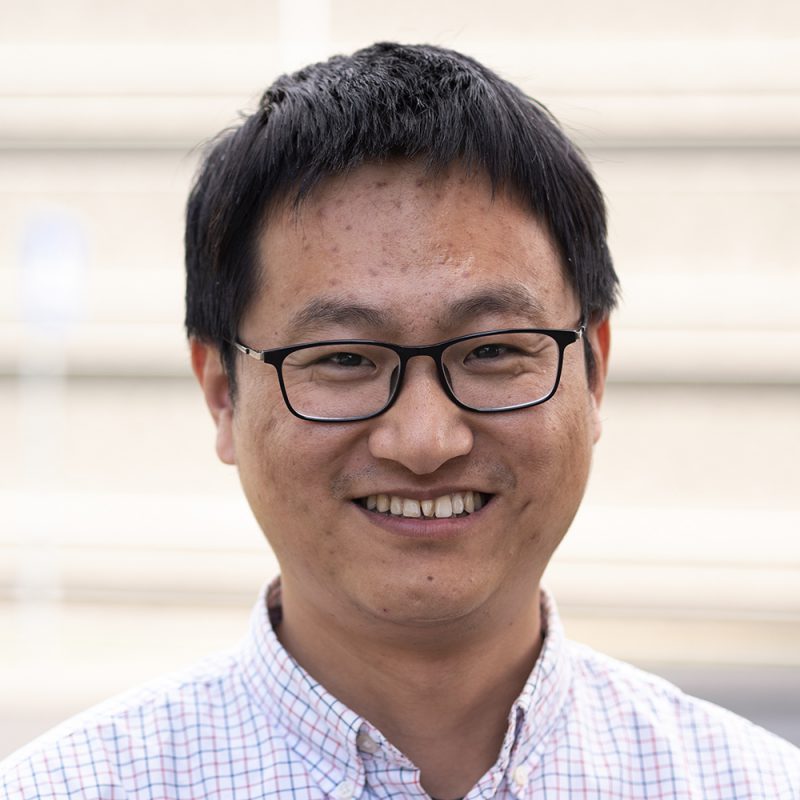
Professor of Cognitive Neuropsychiatry, Head of the Cognitive Neuroscience Center
hallucinations, schizophrenia, apathy, alexithymia, psychosis, psychiatric disorders, suicidality, depression, memory impairment











A major focus of the Aleman group is the cognitive and neural basis of apathy. Patients with psychiatric disorders often experience markedly reduced levels of interest and a lack of initiative in undertaking daily activities, i.e. apathy. Understanding apathy is critical to the welfare of patients because it can severely affect their (social) functioning.
We are studying the neural and cognitive basis of apathy in order to elucidate brain circuits that may be compromised. Specifically, we are investigating how the frontostriatal and frontoparietal circuits are involved in apathy. We are also investigating experimental treatments for apathy, such as repetitive transcranial magnetic stimulation (rTMS), transcranial direct current stimulation (TDCS), and behavioral activation therapy.
Another important focus of the group is the neural basis for predicting the course of major depressive disorder. The effects of preventive cognitive therapy in patients whose depression is in remission are being studied to understand the neurocognitive mechanisms underlying relapse and its prevention in major depressive disorder.
Finally, we are studying the neural basis of suicidality. Suicide is a leading cause of death among young people in Europe, while each year some 25,000 people in the Netherlands need medical care after a suicide attempt. We are studying the cognitive-emotional processes that may be disturbed in people with suicidal tendencies. This research may lead to the development of new treatments.

Aging is an important issue for society, and many people dread the loss of memory and other cognitive abilities that come with growing older. Excessive memory loss can point to early phases of dementia. We are studying the neural basis of mild cognitive impairment (cognitive deterioration that is not yet clinically significant) in elderly people using different neuroimaging techniques. We are particularly interested in the role of apathy as a predictor for dementia. We also aim to improve older people’s cognitive functioning using neurofeedback and neurostimulation.
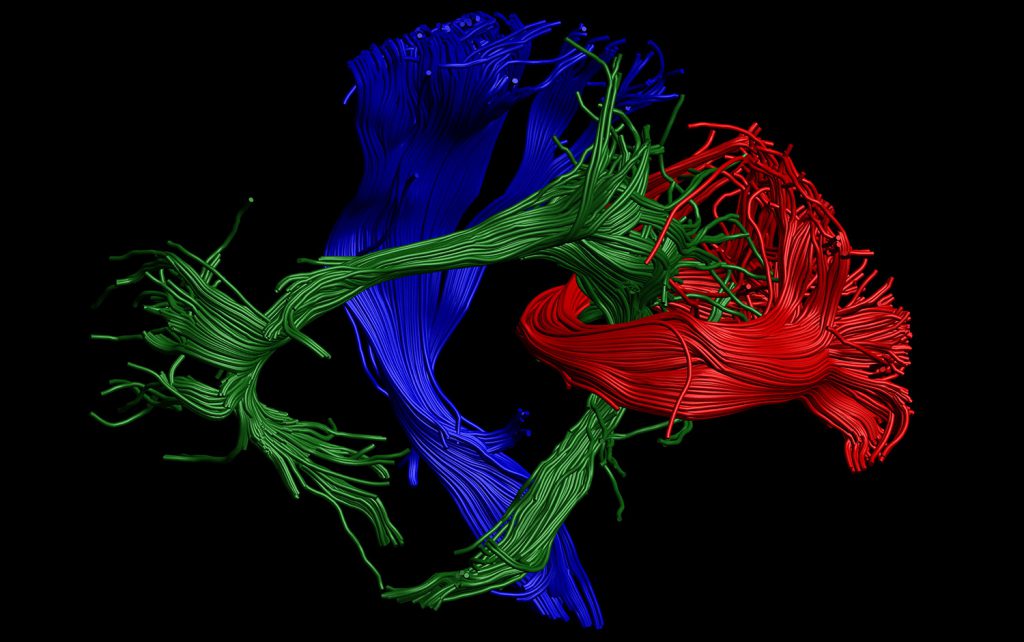
Psychosocial therapies, neurofeedback and neurostimulation are the most important strategies for improving brain functioning. The neural basis of all three is being investigated by researchers in our department. Neurostimulation involves repetitive transcranial magnetic stimulation (rTMS), transcranial direct current stimulation (tDCS), or transcranial alternating current stimulation (tACS).

Update your browser to view this website correctly. Update my browser now